Sussex Premier Health, Hastings: Important update for patients with upcoming appointments
Sussex Premier Health, Hastings: Important update for patients with upcoming appointments
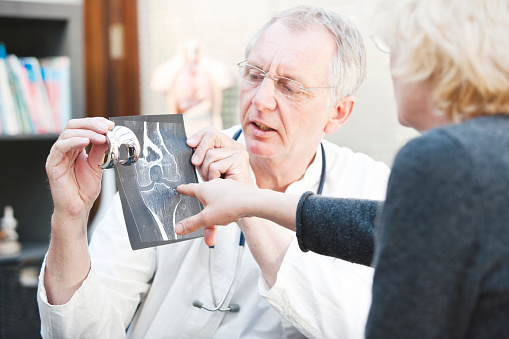
Knee replacement surgery is a critical procedure for those struggling with chronic knee pain or mobility issues caused by conditions such as osteoarthritis. Sussex Premier Health offers private knee surgery in Sussex, combining expert care, clear pricing, and a pathway to recovery designed around you. Below, we’ll explore what the procedure involves, its benefits, the recovery process, and why Sussex Premier Health is the trusted choice for knee joint replacement.
Sometimes know as:
Knee replacement surgery, or knee joint replacement, is a procedure that removes worn or damaged parts of the knee joint and replaces them with an artificial joint. This surgery helps to significantly reduce pain and restore mobility, allowing patients to enjoy a better quality of life.
Knee pain is often caused by:
There are two main types of procedures:
If your knee pain is severe and affecting your daily life despite other treatments, knee replacement surgery might be the right solution for you.
At Sussex Premier Health, you’ll meet your consultant surgeon in one of our private consultation rooms. All our rooms are accessible so there’s no need to worry if walking is difficult for you.
You consultant will ask about your health symptoms and answer any questions you may have. If you haven’t been diagnosed yet they may recommend our diagnostic tests and scans to help them assess your knee in more detail. Both your initial consultation and tests at this stage are charged separately to the cost of any treatment needed.
Your consultant will discuss what would be best for you and your lifestyle and will then advise you about your personal plan and some of the options that are available to you.

On the day of your operation, our ward staff will show you to your own private room. Your private room will have an en-suite bathroom and TV and Wi-Fi facilities.
Once you’re ready, our nurses will help you prepare for your operation. Before your procedure, you will meet with your consultant again and your anaesthetist.
You’ll probably have a general anaesthetic, so you’ll be completely asleep. However, sometimes it’s preferable or necessary to have an epidural (spinal) anaesthetic, where you’re numb from the waist down. If so, your anaesthetist can give you sedatives to help you relax during the operation.
Your consultant will make the necessary incisions and begin to remove worn or damaged areas of your knee joint. They’ll then fit your new knee and close your incisions.
The operation usually takes up to an hour and a half.

A smooth recovery is a crucial part of knee replacement surgery’s success. At Sussex Premier Health, we offer tailored aftercare to support you at every step toward regaining your mobility.
Physiotherapy Support:
Wound Care:
Follow-Up Appointments:
Long-Term Recovery Tips:
Your recovery timeline will vary depending on your age, overall health, and commitment to aftercare activities. On average, most patients resume daily activities within 6 weeks.

At Sussex Premier Health, we pride ourselves on transparent and inclusive pricing. Whether you’re self-funding or using private medical insurance, we make your options clear from the start.

Take the first step towards a life without knee pain. Schedule a consultation with one of our expert consultants at Sussex Premier Health. Whether you’re considering surgery or need advice, we’re here to help. Discover how life-changing knee replacement surgery can be. Your mobility matters—and we’re here to make it better.

You may need a knee replacement at any age, however, getting older increases your risk — those aged between 60 and 80 are most likely to need a knee replacement. Genetics, previous knee injury and lifestyle can also play a part in whether you need a knee replacement, so always seek medical advice if you have symptoms.
Your doctor may recommend knee replacement if:
Knee replacement surgery can relieve pain and help you become more active again. However, you must be healthy enough to undergo surgery.
Your consultant may suggest an alternative to knee replacement, although the results may not last as long. These treatments are often performed using arthroscopy — a type of keyhole surgery using a thin, flexible, telescopic instrument called an arthroscope.
Knee replacement alternatives include:
Your doctor will usually only recommend surgery after you’ve tried other non-invasive alternatives to knee replacement without success. Other treatments include:
Your surgery will be performed by your consultant surgeon.
You’ll be helped out of bed to stand around 12 to 24 hours after your operation. You can then walk with a frame or crutches and should be able to do so independently after a week. If you’ve had keyhole surgery or are on an enhanced recovery programme, it may be sooner.
A physiotherapist will show you some exercises you can do to help strengthen your knee that you can start the day after surgery.
It can take up to two years for your knee to recover, however, you should be able to resume normal daily activities within six weeks and any pain and swelling should settle within three months. Your leg may be swollen for up to a year.
You’ll return to hospital a few weeks after your operation for a follow-up appointment to check your recovery progress.
For most people, their new knee lasts around 20 years or even longer for total knee replacement. Partial knee replacements tend to need to be replaced sooner – after around 10 years. The chances of needing a repeat operation is higher if you’re overweight, you run, play vigorous sports or you conduct heavy manual work.
You should gradually build up any activity, and should be able to manage walking or swimming around six to eight weeks after surgery, depending how fit you were before surgery. You should avoid high impact sports such as running, contact sports or weight lifting. Your consultant or physiotherapist will be able to advise which sports you can do, they may recommend avoiding tennis, squash and skiing, but cycling, dancing and golf may be fine.
Preparing for your surgery by being as fit as possible and strengthening your knee muscles will help improve your recovery time. Before your operation, it’s also a good idea to prepare your home to make it easier for you to get around safely and more easily. Remove anything you can trip over and make sure important items are easy to reach.
For the first few days or weeks at home, you may need someone to help you with errands and household chores.
Speak to your consultant or GP before flying to find out what’s right for you. It’s important to note that your chance of deep vein thrombosis (DVT) increases if you fly after recent surgery.
Airlines have their own regulations about passengers flying after surgery, so make sure you check beforehand.
Knee implants are made from high-grade plastics, polymers and metal alloys.
There are several different metals commonly used in knee replacements, specifically cobalt-chromium, nickel, titanium and zirconium.
Yes, both knees can be replaced at the same time. This may be recommended if you have osteoarthritis in both knees. However, the surgery and recovery time are longer — you will also need more support during your recovery.
Yes, you can have a knee replacement if you are overweight. However, being overweight puts you at greater risk of certain complications during and after surgery. Your doctor will discuss the benefits and risks of knee replacement surgery in your particular case with you so you can make an informed decision.
Speak to a member of our team